April 25, 2024
The first case of living donor liver transplantation using the right posterior section for a patient with haemophilia
Nagasaki University Hospital (Hospital Director: Makoto Osaki) performed a living donor (in his 30s) liver transplantation using the right posterior section on February 28, 2024 for a hemophilia patient (male in his 60s) with hepatocellular carcinoma and type C cirrhosis. Patient was successfully discharged on postoperative day 47.
|
The organ to be transplanted is called the graft. |
 |
Hemophilia is a disease in which the blood clotting factor is deficient or absent. Once bleeding occurs, it takes a long time for stop bleeding, and it can lead to anemia and hemorrhagic shock. In addition, liver transplantation is one of the most highly invasive surgical procedures and carries a high risk of massive bleeding, so liver transplantation for hemophilia patients requires particularly careful blood coagulation management. Therefore, in this surgery, we were able to safely perform the operation by adopting the accurate intraoperative coagulation capacity evaluation and preoperative and postoperative management methods for hemophilia patients, which were the results of research conducted by the MHLW Research Group on liver transplantation in patients with multiple infections using blood products (Principal investigator: Susumu Eguchi, Nagasaki University Graduate School of Medicine, Co-researcher: Professor Tetsuya Hara of the Department of Anesthesiology).
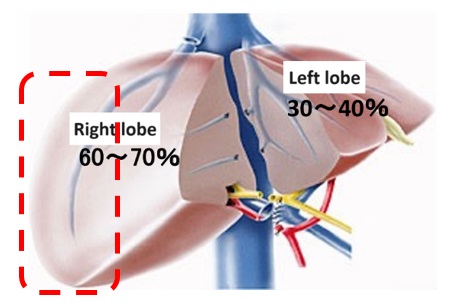
In living donor liver transplantation, careful consideration must be given to the size of the donated liver to ensure donor safety, but by using the right posterior section, a safe volume of liver could be left for the donor, presenting a new option in living donor liver transplantation, where previously only the right or left lobe was available. The living donor was discharged from the hospital on the 8th day after surgery and has already returned to daily activity.
Providing liver transplantation as a treatment option for hemophilia patients with type C cirrhosis and hepatocellular carcinoma directly improves the quality of life of hemophilia patients. We hope that this procedure will be widely recognized by society and become established as a new surgical procedure.










